Hypnobirthing: Science-backed relaxation for positive birth outcomes
/Hypnobirthing: it sounds so airy-fairy that I can almost hear the collective scoff of the Obstetric Old Boys’ Club, but more and more research is amassing in support of self-hypnosis for a calm, empowering birth experience, requiring little or no medical intervention. Studies have connected Hypnobirthing practices with shortened labour, reduced pain and discomfort, and lower rates of caesarean section, gas, and epidural.[i][ii] Possibly the best part about Hypnobirthing is that the power to achieve these outcomes is entirely in your hands, taking the power away from health professionals and putting YOU at the centre of your birth – calm, in control, and fully aware of how your body is working for you and your baby in each stage of labour.
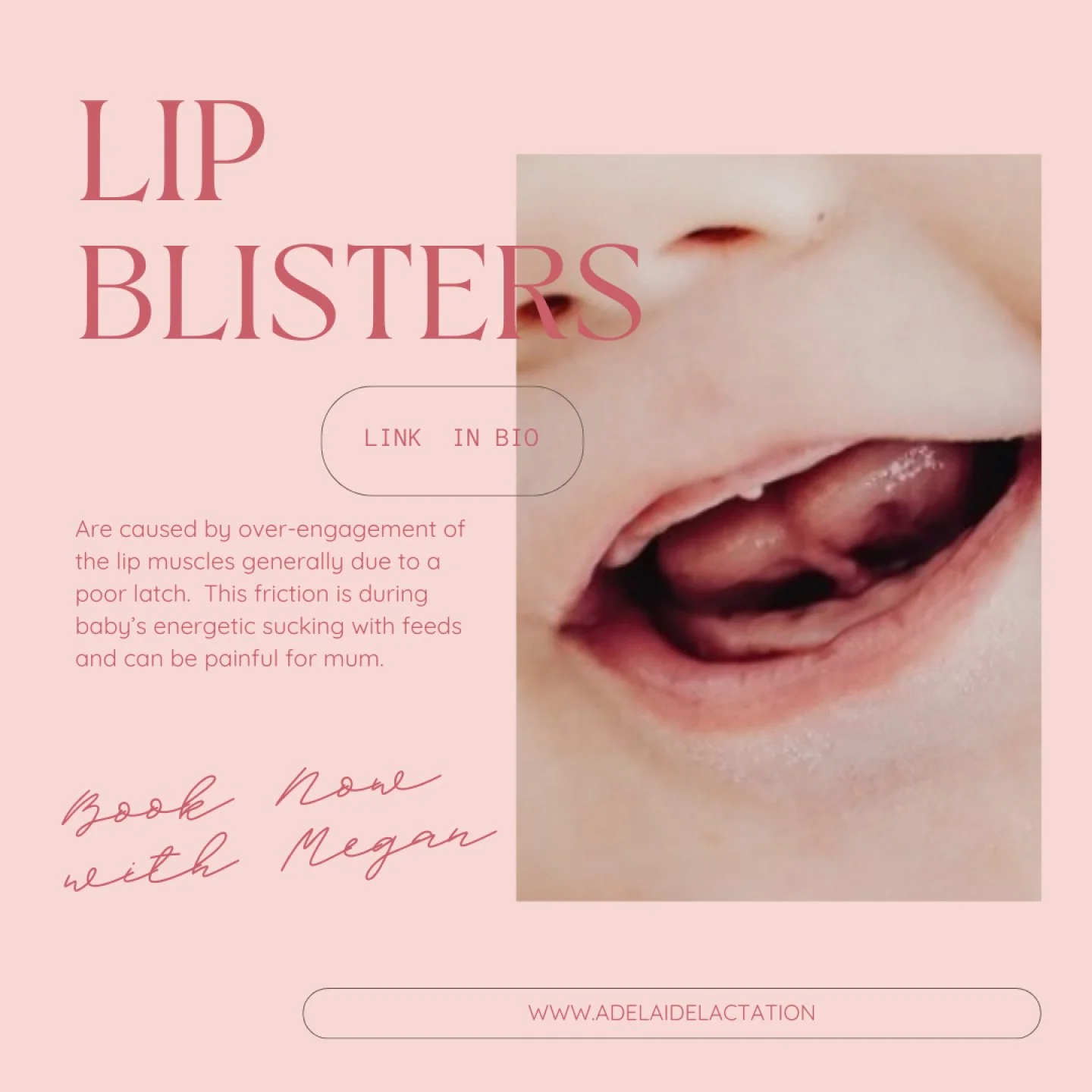
But what is Hypnobirthing exactly, and how does it achieve the kind of unicorn birth that many women envision? Hypnobirthing is based on the premise that women can use the power of the mind to work with the natural flows and rhythms of their labouring bodies, trusting their bodies to function as nature intended, rather than fearing the unknown and the potential for pain. It does this by educating women and their birthing partners about the stages of labour and what the body does at each stage; as well as self-hypnosis techniques, like breathwork, to manage fear, stress, and pain; and the ways in which birth companions can support the birthing woman. Women’s satisfaction with labour increases when they have low levels of fear and pain[iii]; receiving care that aids in their relaxation reduces fear and aids positive birth outcomes.[iv] Hypnobirthing will give you confidence that the peaceful, drug-free birth you hope for isn’t so mythical.
Hypnobirthing is usually delivered in-person, across four, three-hour sessions, with a registered practitioner, with online options also available. You and your birth companion will learn the theory that informs Hypnobirthing, including how your hormones assist the process of labour and birth, the role of fear and stress in your perception of pain, and the power of your mind in overcoming fear. Together, you’ll practice self-hypnosis techniques, such as meditation, acupressure, massage, and deep breathing so that these practices are second nature by the time you go into labour. The ideal time to complete your Hypnobirthing course is when you are between 20 and 30 weeks pregnant, to help you feel at ease about your baby’s birth and give you ample time to hone your new skills. But if you’re late to the party, you will absolutely benefit from learning about Hypnobirthing, even very late in pregnancy.
To understand why Hypnobirthing achieves such positive outcomes, it is useful to first look at the consequences of common birth interventions and the environment in a hospital birthing unit, and how these impede the natural processes occurring within mum’s body to facilitate a healthy birth. Normal term, spontaneous labour and birth is the culmination of a complex dance of hormonal processes, signifying the physical readiness of baby to be born and mum’s physical readiness to birth. While there is a normal, gradual rise in maternal stress hormones during labour, which should peak towards the end to aid baby’s expulsion, excess fear, anxiety, or pain throughout labour, and associated surges in stress hormones, can result in decreased frequency or intensity of contractions.[v]
One stark example of this is the tendency for labour to stall once the labouring woman arrives at hospital, as she adjusts to her new surroundings. What is comfortable and familiar to health staff might be the birthing woman’s fluorescently-lit hellscape, equipped with intimidating medical apparatus and domineering birth attendants, who encourage her to labour on her back, withhold food, and time-keep her labour to a rigid schedule. If labour fails to progress in accordance with standardised modelling, a cascade of interventions is sometimes introduced, including overzealous electronic fetal monitoring, artificial membrane rupture, and the administration of syntocinon, to intensify contractions.
Contrast the above scenario with Hypnobirthing’s emphasis on dim lighting, soft music, positive affirmations, aromatherapy, visualisations, massage, breathwork, freedom of movement, and limited intervention, pending a clear medical need, and it’s not difficult to see how a comfortable, relaxing, and empowering environment might help the birthing woman manage fear, stress, and pain, even in situations where some level of medical intervention is needed.
Despite growing awareness of the impact of natural birthing methods, like Hypnobirthing, and more parents desiring a peaceful, unhurried, and unimpeded birth experience, medicalised birth persists. Australia’s caesarean section rate is exorbitantly high at around 34% of births, despite the World Health Organisation advice that 10-15% is an ideal caesarean rate. Inductions are commonplace, with a trend towards scheduling them well ahead of women’s estimated due date. Many women are told that they will need to be induced or schedule a caesarean if they have not gone into labour by their due date, despite the fact that an estimated due date is just that – a guess – and a healthy pregnancy should be allowed to progress to 40 weeks and 10 days.
When elective induction is chosen, with no medical basis, this correlates with an increased need for pain relief, epidural anaesthesia, instrumental delivery, and caesarean delivery for mum, and possible low birthweight, shoulder dystocia, neonatal resuscitation, and admission to the neonatal intensive care unit for baby.[vi] Syntocinon, which is given to chemically induce or speed up labour, can intensify contractions and labour pain quite suddenly, and limit your ability to manage pain through Hypnobirthing.
Choosing a supportive birth attendant is vital. Asking the right questions of your midwife or obstetrician from your first meeting will ensure you have a true partner in the birth you desire and deserve: do they embrace Hypnobirthing and natural birth? What are their thoughts on induction? What is their caesarean rate? What will they recommend if you haven’t gone into spontaneous labour by 40 weeks? What interventions do they routinely use during labour? Are they supportive of limited birth interventions? Will they welcome and respect your birth plan? Do they have any leave booked around your estimated due date? Are they happy for you to labour and birth in any position that feels comfortable? Are they happy for you to labour in water or spend time outside of the birthing suite? Do the hospitals where they practice welcome Hypnobirthing methods? Ask for their stats. It’s a good idea to vet the hospital you wish to birth at, too, and make sure their birthing suites are compatible with your birth plan.
We offer Hypnobirthing classes in the South of Adelaide for couples seeking education. For the highest quality Hypnobirthing education, be sure to visit the Hypnobirthing Australia ™️ website[VR1] , where you’ll see my face on the certified practitioners page. Here, you can search for a practitioner in your area, or sign up for an online course. I wish you all the very best for a safe, calm, and empowering birth.
To book into an Adelaide Hypnobirthing & Childbirth Education class in person/online - book here
Megan x
[i] Phillips-Moore, J 2013, ‘Birthing outcomes from an Australian HypnoBirthing programme’, British Journal of Midwifery, vol. 20, no. 8, pp. 41-42.
[ii] Swencionis, H, Rendell, S, L, Dolce, K, Massry, S, & Mongan, M. 2012, ‘Outcomes of HypnoBirthing’, Journal of Prenatal and Perinatal Psychology and Health, vol. 27, no. 2, pp. 120-139.
[iii] Khresheh, R 2010, ‘Support in the first stage of labour from a female relative: The first step in improving the quality of maternity services’ Midwifery, vol. 26, no. 6, e21. https://doi. org/10.1016/j.midw.2008.11.03
[iv] Hodnett, E, D, Gates, S, Hofmeyr, G, J, & Sakala, C. 2013, ‘Continuous support for women during childbirth’, The Cochrane Database of Systematic Reviews, vol. 7, pp. 1-20. https:// doi.org/10.1002/14651858.CD003766.pub5
[v] Alehagen, S, Wijma, B, Lundberg, U & Wijma, K 2005, ‘Fear, pain and stress hormones during childbirth’, Journal of Psychosomatic Obstetrics and Gynecology, vol. 26, pp. 153-165.
[vi] Goer, H, Leslie, M, S & Romano, A 2007, ‘The Coalition for Improving Maternity Services: Evidence basis for the ten steps of mother-friendly care: Step 6: Does not routinely employ practices, procedures unsupported by scientific evidence’, Journal of Perinatal Education, vol. 16, no. 1, pp. 32S-64S.
[VR1]Add link to blog: https://hypnobirthingaustralia.com.au/directory/